Urinary Incontinence in Women- Causes, Symptoms and Treatments
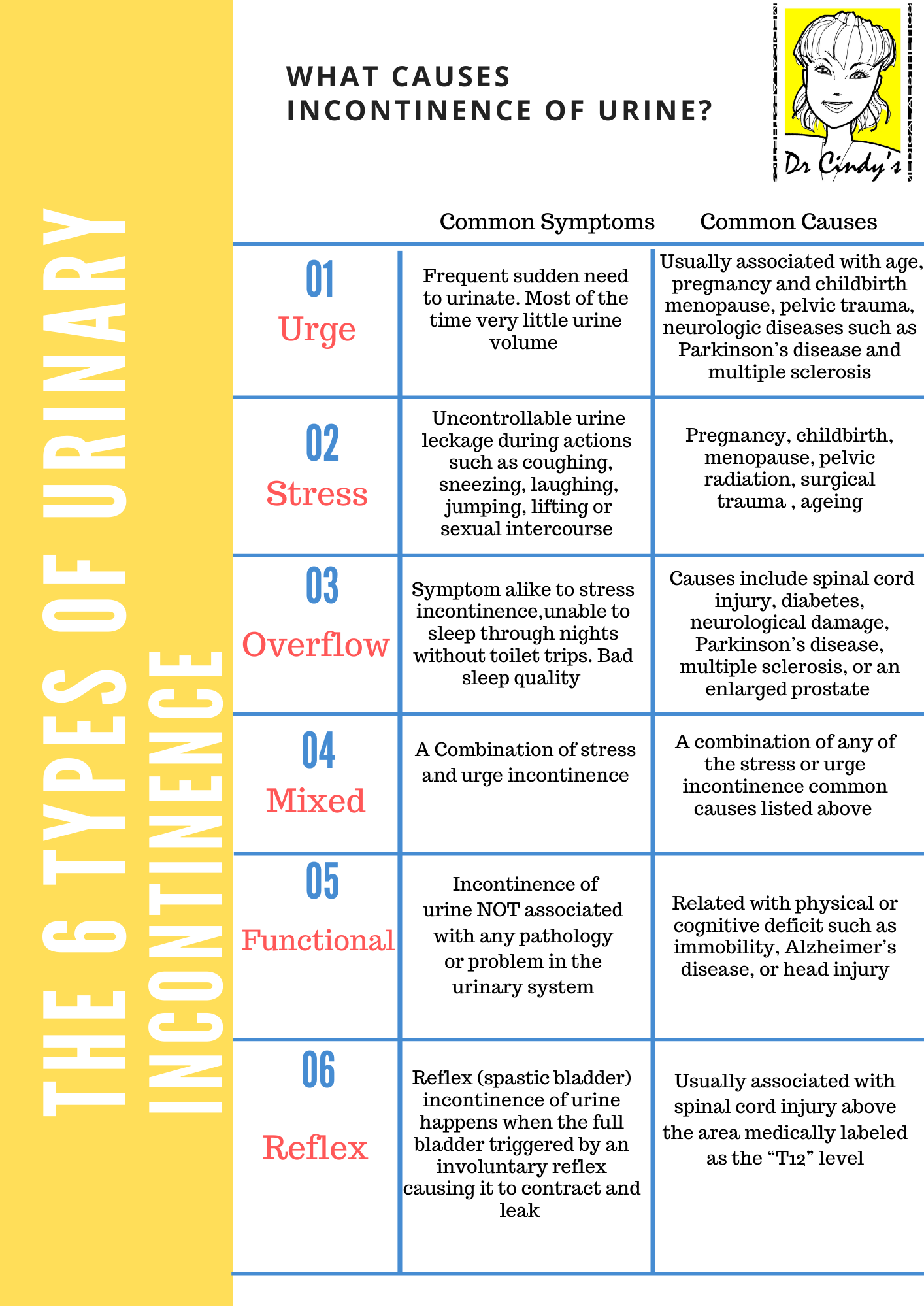
Dr Cindy was chatting with a regular patient about her aesthetic treatments when the topic of exercising came up. Almost tearing she reveals: “I am not trying to exercise to lose weight, I am trying to exercise because I want my vaginal muscles tighter and more importantly, I want to stop my urine leaking out!”. The patient went on to describe how her urine leaks when she sneezes, and when she tries to lift things. In the last five years, her sleep quality was not good as she wakes up 2 to 3 times nightly for toilet trips. Nights when she was too tired and ignored the urge, she could end up wetting her bed. Sanitary pads become a daily necessity for her, and she always imagines she smells bad. It was also tricky for her to discuss this issue with anyone, not even her husband. These are common symptoms of Urinary Incontinence in Women.
This encounter that Dr Cindy first had with her patient many years ago has become an oft-repeated story that Dr Cindy hears from many other patients since. Urinary incontinence in women is a common issue many women experience after age 45, as life’s journey through natural childbirth, sedentary lifestyle, weight gain and hormonal changes bring about this deterioration in the pelvic tissues. It is not just the outward signs of ageing in the face and neck, significantly the body also goes through a tremendous ageing process, losing tautness, and leading to vaginal laxity and overall looseness at the genital area. The standout issue of this body ageing is urine incontinence, which can become an overwhelming personal problem in facing society.
Physiological Treatments
Physiological treatments are simple, do-it-yourself exercises at home, with no adverse effects. These treatments can be used in combination with other therapies, work well for certain types of incontinence, and are useful for many women.

Urine leak caused by simple actions such as lifting or sneezing. One always feel the sense of urgency even the last toilet trip was only minutes ago. It can be embarrassing and frustrating.
Physiological treatments include:
Bladder Training
The purpose of bladder training is to control the urge and regain the control of the bladder, extending the intervals between emptying urinating and increasing the amount of fluid your bladder can hold. This method entails scheduling bathroom visits at set times during the day, for example, every 90 mins. This training can help reduce the sense of urgency and leakage.
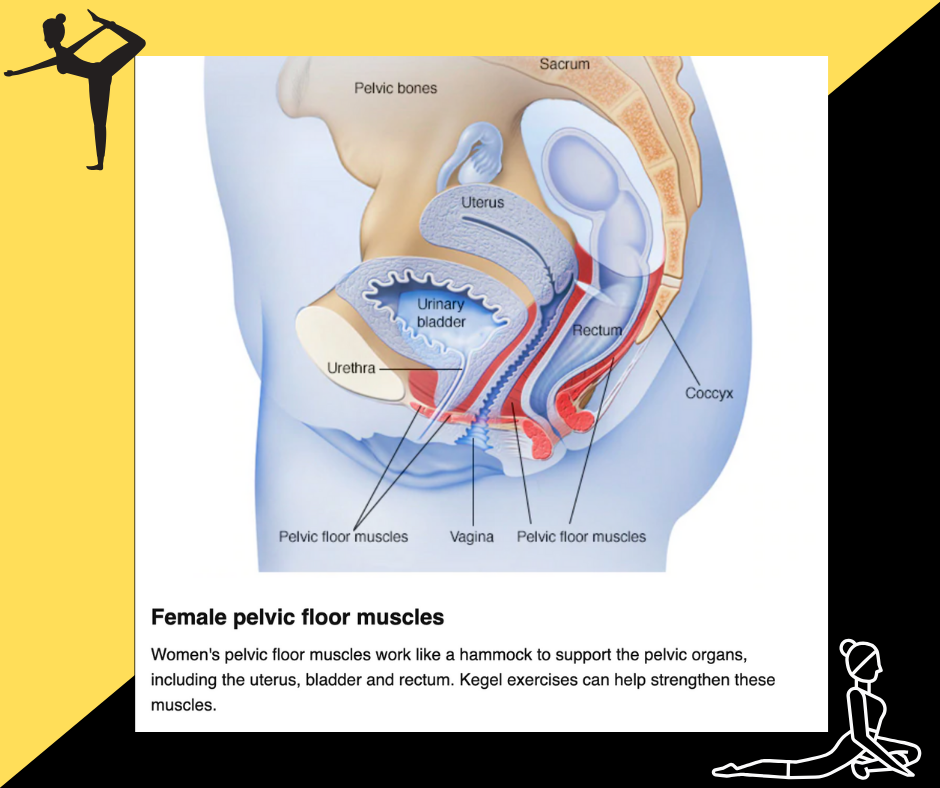
Daily pelvic floor exercises
Pelvic muscle exercises, also known as Kegels, can be effective at reducing leakage, but it’s essential to do the exercises correctly. They are an indispensable part of improving Urinary Incontinence in Women, preventing it from getting worse, and helping you suppress the urge to urinate. You can feel your pelvic floor muscles when you “try to stop the flow of urine” during voiding. To build your pelvic floor muscles, sit comfortably and squeeze the muscles in a set of 10 to 15 times.
These exercises strengthen and tone the muscles that support the pelvic wall. Results come to those who persevere, as it requires a firm commitment to doing their sets regularly. Correct technique is crucial. Unfortunately, some women cannot locate their pelvic floor muscles or are unable to persevere with the Kegel exercise routine, and hence find this training difficult and not achieving improvement.
Quit smoking and cut down on alcohol
Smoking increases the risk of urine incontinence because coughing (smokers’ cough) puts a strain on your pelvic floor muscles. It is also no secret that smoking is never good for any aspect of health. Programmes to help you quit smoking in Singapore is available from Singapore health promotion board https://www.healthhub.sg/programmes/88/IQuit. You can also ask your doctor or pharmacist about the programs available.
Alcohol is a diuretic that makes you urinate more often. Cutting down or quitting may help your urine incontinence symptoms. Urinary Incontinence in Women can be aggravated with regular alcohol intake
Avoid lifting
Lifting strains your pelvic floor muscles, so avoid it wherever you can. When you perform lifting actions, such as picking up children or carrying shopping bags, try to tighten your pelvic floor muscles before and during the lift.
Avoid Obesity
Being overweight means increased pressure of fatty tissue on your pelvic floor muscles and bladder. This increased pressure is akin to continually squeezing on the bladder, leading to increased risk of leaking. Urinary Incontinence in Women may improve and could clear up with the ideal body weight.
Increase water intake and decrease coffee drinking
Caffeine can irritate the bladder for some people and thus makes urinary incontinence worse. Try switching to decaffeinated coffee. Take note that carbonated drinks such as cola and sprite, tea and cocoa also contain caffeine, and it will be better to replace them with water, herbal or fruit teas.
People with urinary incontinence sometimes tend to avoid drinking fluids as they feel it causes more toilet trips. However, reducing your fluid intake makes urine incontinence worse because it reduces your bladder’s capacity. However, if there are medical conditions that may require you to limit your fluid intake; your doctor will advise you on this.
Biofeedback
Biofeedback will help patients who find it challenging to locate the pelvic floor muscles because they cannot see this set of muscles and are unable to determine if they are doing pelvic muscle exercises correctly. Biofeedback therapy uses computer graphs to show you the muscles you are exercising by attaching two sensors on the genital area, allowing the training therapist to direct your exercise and measure your muscle strength. Biofeedback also allows your therapist to design a personal exercise program for Urinary Incontinence in Women, that can help you learn to control and strengthen your pelvic floor muscles, which play an essential role in bladder control.
Medications
Estrogen replacement therapy in oral form or skin patch form is not an adequate treatment for female urinary incontinence. Some vaginal estrogen in different methods such as vaginal rings, vaginal pellets, or creams has helped reduce recurrent urinary tract infections in postmenopausal women. Still, their effectiveness for urge incontinence is unknown. Medications like pseudoephedrine are sometimes used to help tone up the urethra and can improve stress incontinence. Other types of medicine can help to relax a hypertonic bladder. They can be used on its own or in combination with physiological treatments. https://www.webmd.com/urinary-incontinence-oab/4-medications-that-cause-or-worsen-incontinence
These medications can help in reducing problems of bladder control, but they cannot cure urge incontinence.
ThermiVa®
ThermiVa® is an entirely non-surgical procedure that does not require anaesthesia and has no downtime. This painless, non-surgical treatment uses radio-frequency (RF) energy which helps tighten the underlying mucosa and supportive tissues of the vagina, pelvic muscle wall, urethra and tissues beneath the bladder. ThermiVa® stimulates natural collagen production and tissue rejuvenation by transmitting gentle thermal energy for incontinence treatment. Women see improvement in the appearance of external female genitalia from one session, and they will experience better urinary control, tighter vagina walls, improved lubrication, better vaginal sensation leading to heighten orgasms. Three sessions of ThermiVa®, each treatment being one month apart, after which this treatment can last up to 18 months. ThermiVa® is sufficient on its own, but a combination program of thermiVa® with a functional magnetic therapy, Tesla Care Device, gives enhanced results.
Tesla Former Care Device
The Tesla Former Care Device is primarily for the training of the pelvic floor muscles and treatment of urinary incontinence using the unique FMS technology – Functional Magnetic Stimulation. It delivers electromagnetic fields to the peripheral nerve in your body, which triggers your motoric nerves. This FMS stimulation causes your muscles to contract and relax. FMS uses super inductive properties of the magnetic field deep inside the body and thus stimulates muscles that one cannot reach using electrical stimulation. To improve Urinary Incontinence in Women, it will be a more natural way to discover your kegel muscles compare to biomodelling. The pulsed magnetic field generated by the Tesla Former Care device causes the muscles of the pelvic floor to contract without the need for any electrodes. Tesla FMS treatment increases the strength and endurance of the pelvic floor muscles by delivering 50,000 contractions in 30 minutes! One can sit through the treatment sessions fully clothed on the tesla chair, which has two in-built applicators for precise targeting of areas.
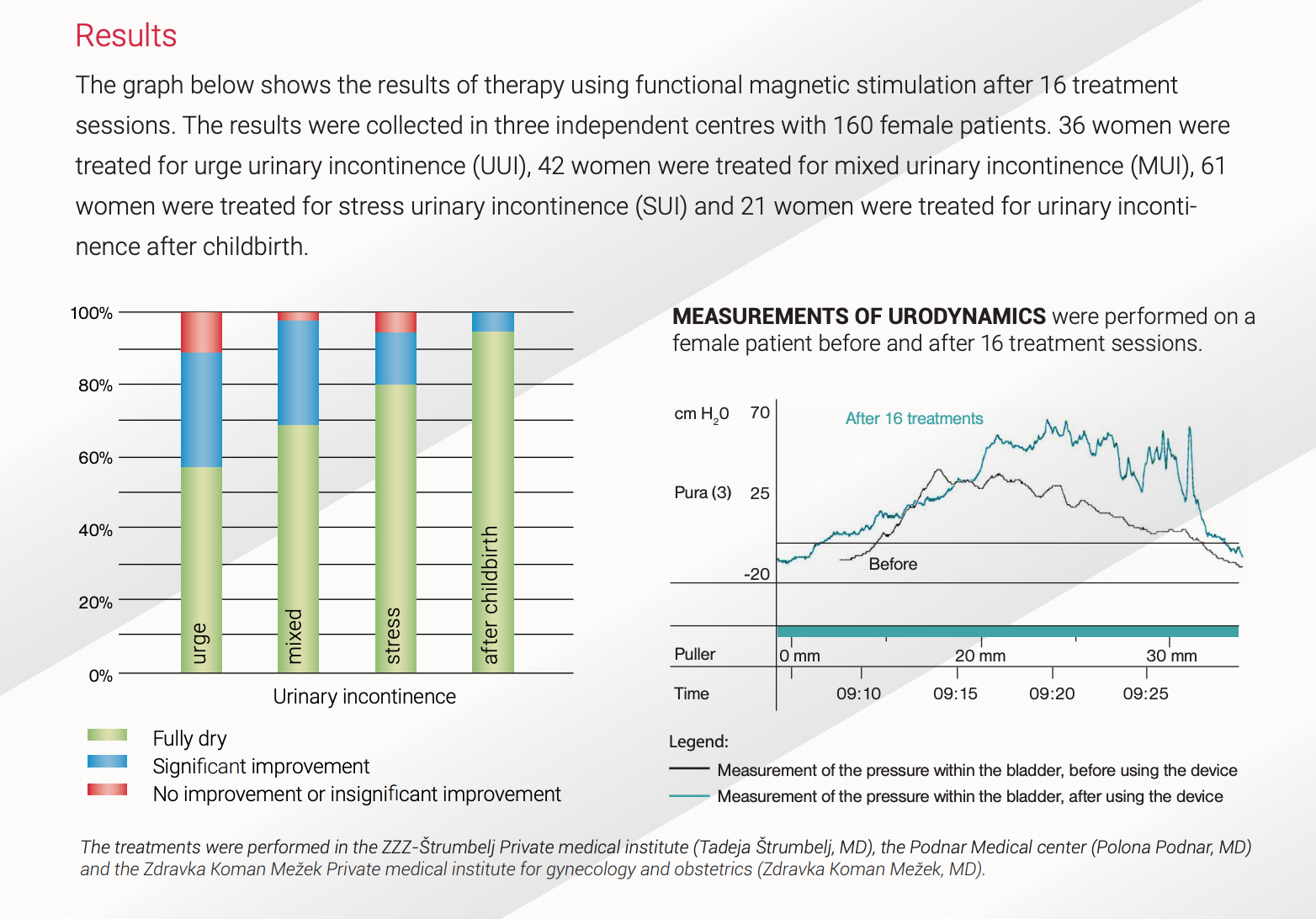
The graph below shows the results of therapy using functional magnetic stimulation after 16 treatment sessions.
Sacral Neuromodulation Therapy
Sacral neuromodulation therapy applies electrical impulses directly to the sacral nerves. Doctors thread wires through openings in the pelvic bones along the sacral nerves. This procedure is done in an operating room using local anaesthesia. The cables are attached to a small external generator. A two-week stimulation test using the external device to determine suitability and improvement in incontinence symptoms, measured to be at least 50% and above The implant of the sacral nerve stimulation neurostimulator will only take place if the requirements are met in the first phase. The 2nd procedure is short, performed under general anaesthesia. The neurostimulator typically lasts for 5-10 years and will need to be replaced, usually during an outpatient procedure.
Botox Bladder Injections
When Botox is mentioned, people automatically think of wrinkle-smoothening, but Botulinum toxin A is a medical substance that can help to control spasms, reduce sweaty palms and underarms. In this case, doctors use Botox to treat patients with urge incontinence by paralysing bladder muscle, reducing unwanted bladder contractions.
Botox is injected into the muscle wall of the bladder under local anaesthesia. Maximum relief is usually seen seven days after injection and lasts typically six to 12 months. Repeat injections are needed at between 6 to 12 months interval. A downside of bladder Botox is patients cannot empty the bladder on their own, with residual urine that might lead to the possibility of bladder infection.
There is no complete cure to Urinary Incontinence in Women, seek early treatment to prevent the condition from deteriorating. Please do not suffer in silence, speak to a doctor to discuss the medical options available.

 14 Jun 2020
14 Jun 2020